Powered
by Paolo
Platania,best
view at 1024 x 768, first issued gen 29 2007, contents editing in
progress, last update of this page dec 16 2008
Posture, etiology of a syndromePaolo
Platania
|
Posturology
guidelines and
interdisciplinary case study |
||||||
|
|
|
|
Posturology
|
The case study
|
The backstage
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Evidences
Platania's syndrome relevant findings grouped by classes:- Clinical evaluation findings: everything that may be assessed by external observers;
- Symptomatic and degenerative findings: resulting from pain sensation, uneasy sensation or completely asymptomatic but confirmed by lab exams;
- Self evaluation: motor disorders that may be fully assessed by internal observers (patient) and only partly evident to external observers;
- Regression events: precious finding, thoroughly described;
- Orthodontic treatment, outcome and followup: description of the treatment and relationship with the above evidences.
| EVIDENCES: clinical evaluation findings | |||||
| # | Finding | Images & details | |||
| Ecl01 | Left ankle: slighty pronated | No image | |||
| Ecl02 | Left soleus (S): contracted, hypertrophic | ||||
| Ecl03 | Left hip adductor: contracted | No image | |||
| Ecl04 | Left tensor fascia lata (TFL) and rectus femoris (RF) : contracted, hypertrophic | ||||
| Ecl05 | Gluteus maximus (GM): inhibited | Inhibited with habitual pelvis pathologic tilt
 click to enlarge |
Tonic with forced pelvis physiologic tilt
 click to enlarge |
||
| Ecl06 | Hamstring: inhibited | No image, palpation evaluation | |||
| Ecl07 | Left hip: medially rotated | Habitual unilateral left hip pathologic
medial rotation, hands fall asymmetrically
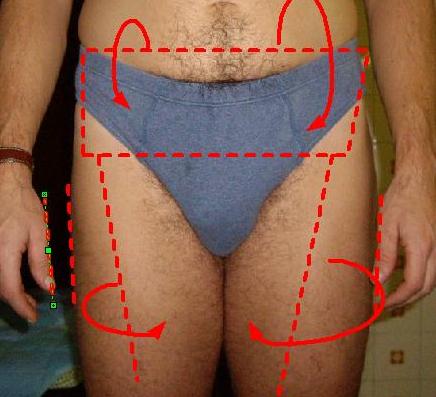 click to enlarge |
Forced bilateral hip physiologic rotation,
hands fall symmetrically
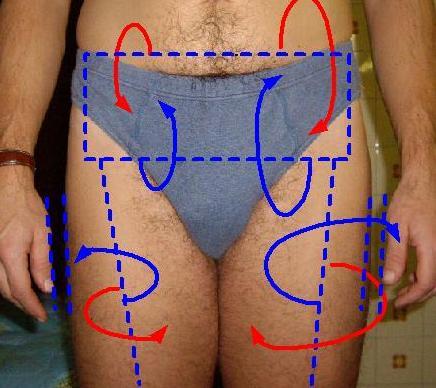 click to enlarge |
||
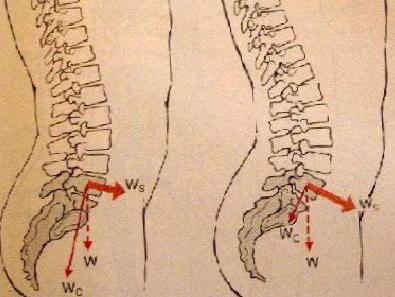
| Ecl08 | Pelvis: anterior tilted | Courtesy of Carol Oatis "Kinesiology: the mechanics and pathomechanics of human movements": left physiologic pelvis tilt as opposed to right pathologic anterior tilt lamented by the patient, see also Ecl04, Ecl06. | |||
| Ecl09 | Penis: right curved | No image | |||
| Ecl10 | Left internal oblique (IO): contracted | ||||
| Ecl11 | Right abdominal and chest hair: less thickness | ||||
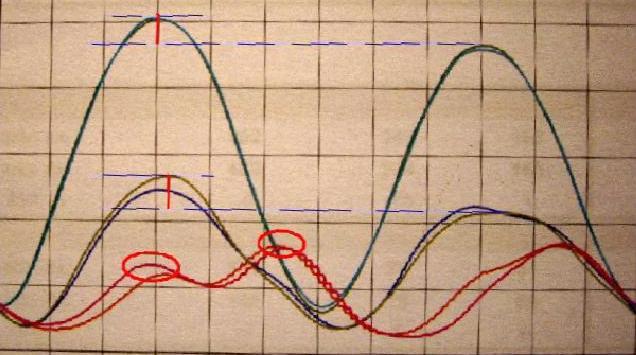
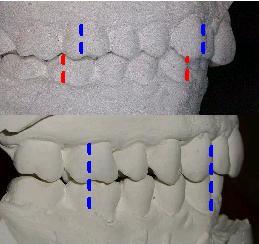
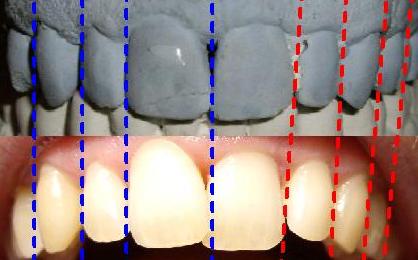
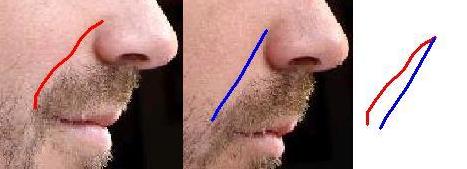
| Ecl12 | Spine curves: increased lumbar lordosis, increased dorsal kyphosis | Differential evaluation: red ordinary pathologic curves, blue more physiologic curves due to induced mandible slight protrusion by bite cotton thickness appliance | |||
| Ecl100 | Left erector spinae (ES): inhibited | No image, self evaluation | |||
| Ecl13 | Left pectoralis major (PM) (clavicular portion): hypertonic | Courtesy of Henry Grey "Anatomy of the human body"
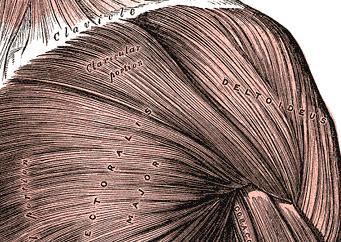 click to enlarge |
reduced scapular abducted lateral rotation ROM due to hypertonic PM
 click to enlarge |
normal scapular abducted lateral rotation ROM
 click to enlarge |
|
| Ecl14 | Shoulder girdle: forwarded | Differential evaluation: left pre orthodontic humeral convergence, right post orthodontic humeral divergence | |||
| Ecl15 | Left shoulder: scapulohumeral joint (SHJ) further forwarded | forwarded SHJ increased adducted medial
rotation range of movement (ROM)
 click to enlarge |
less forwarded SHJ normal adducted medial
rotation ROM
 click to enlarge |
||
| Ecl16 | Left scalenes: contracted | 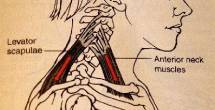 |
Courtesy of Carol Oatis "Kinesiology: the mechanics and pathomechanics of human movements" | ||
| Ecl101 | Left splenius capiti (SC) and trapezius (T): contracted | No image, palpation evaluation | |||
| Ecl17 | Cervical spine: forwarded | Courtesy of Carol Oatis "Kinesiology: the
mechanics and pathomechanics of human movements"
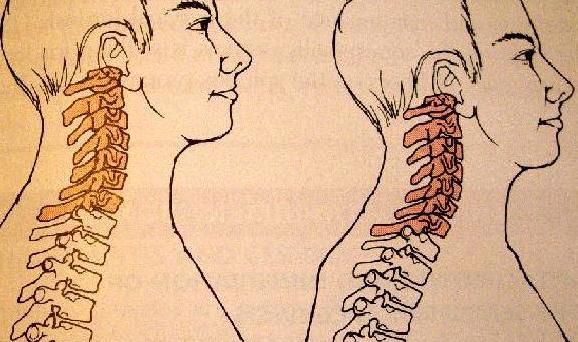 click to enlarge |
|||
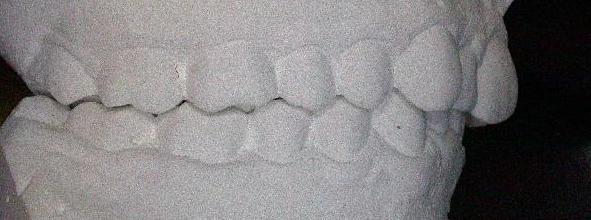
| Ecl18 | Temporomandibular joint (TMJ): retruded | ||||
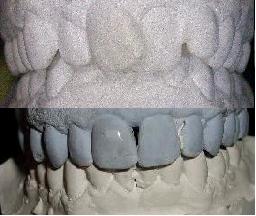
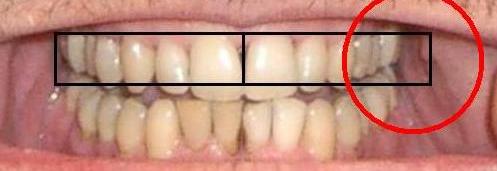
| Ecl19 | Bite occlusion: distocclusion II class II division, incisors crowding, deep bite, mandibular wisdom teeth extrusion over the bite plate, maxillary wisdom teeth extrusion under the bite plane, lack of canine and incisor guidance | ||||
| Ecl20 | left emitongue: weak | Protruded tongue deviation is a neurological indicator of unilateral weakness effecting the side the tongue deviates to | |||
| Ecl21 | Palate: velopharynx asymmetry | ||||
| Ecl22 | Left maxillary arch: insufficiently expanded | After orthodontic therapy, the "before" situation doesn't allow reliable inter incisors line location to evaluate the arches asymmetry | |||
| Ecl23 | Cheek and lips muscles: contracted | Differential evaluation: red ordinary pathologic mimic expression, blue forced expressionless | |||
| EVIDENCES: self evaluation | |||
|
Findings reported by the patient, assessed by means of self analysis and self designed test generic co-contraction test: the co-contraction disorder is easily assessed by an operator rapidly and randomly flexing and extending the involved joint having the patient resisting the action, he will not find any resistance in the first degree of each direction change (lack of underlying co-contraction) but only after a slight delay (eliciting antagonist voluntary contraction); ankle co-contraction test: the co-contraction disorder is easily assessed with the shoe wearing task where the patient attempts to wear a shoe without using hands, the foot has to sneak in the shoe using toe and ankle deformations by co-contraction of tibialis anterior (TA) / tibialis posterior (TP) as well as extensor hallucis longus (EHL) / flexor hallucis longus (FHL) and extensor digitorum longus (EDL) / flexor digitorum longus (FDL); difficulties in the task may underline co-contraction disorder; genioglossus (GG) contraction test (Ese08): put a stick in the mouth having one end deep (as deep as possible) in the mandibular sub-lingual cavity and the other free outside the mouth, pulling vertically using pre molar teeth as fulcrum and having the patient exert as much tongue depressing torque as possible it is possible to manually test the GG force. Maximal torque left-to-right-side unbalance supports unilateral tongue weakness. |
|||
| # | Finding | Images & details | |
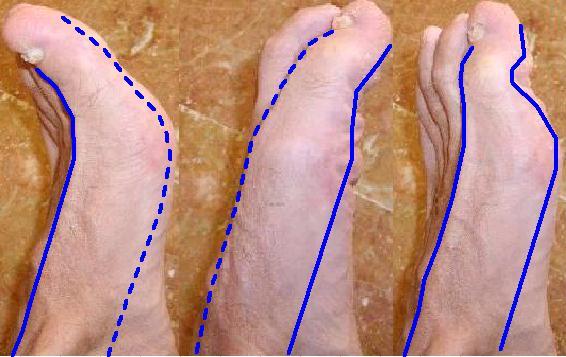
| Ese01 | Left hallux: motor disorder | Inhibited co-contraction of extrinsic foot muscles extensor EHL and FHL, resulting in
impossibility to voluntarily flex the first phalangeal joint (PJ),
furthermore, visibly low EHL basal contraction (EHL tendon not tight), slight
improvement with specific exercises; the finding is further supported by generic co-contraction test applied to
big toe first phalangeal joint. Solid blu line in the image represent tendon activated by concentric muscle contraction, dashed blu line represents passive tendon due to muscle inhibition. This condition is harmful because leads to ingrown big toe nail: inability to flex the big toe during swing phase of gait causes EHL to extend a straight big toe having its nail excessively pushing against the shoe. |
|
| Ese02 | Left intrinsic foot muscles: muscular spasm | Systematic intrinsic muscle spasm (cramp) during left foot unresisted toes flexing, supposed reason is the unresisted flexing torque (due to lack of extensors muscle basal tone) causing muscle to cotract close to minimum length excursion range, cramps subside with passive toes hyperextension. | |
| Ese03 | Left ankle: motor disorder | Inhibited co-contraction of tibialis anterior (TA) and tibialis posterior (TP) to control and stabilize the foot resulting low plantar arch (slight pronation), unsteady motion and pathologic motor compensations (alternative muscular firing pattern) and ankle joint degeneration, the finding is further supported by ankle co-contraction test. | |
| Ese04 | Left hip: motor disorder | Inhibited posterior thigh muscles semimembranosus (SM), semitendinosus (ST), biceps femoris (BF), GM due to overactive TFL and RF, resulting in poor coxofemoral joint stabilization, pathologic motor compensations (alternative firing muscular pattern) and joint degeneration; the finding is assessed by generic co-contraction test applied to left hip joint. | |
| Ese05 | Postural cycling analysis | The chart, resulting from instrumental cycling evaluation, perfectly assists in describing the self evaluated motor unbalance during cycling activity and its harmful features: at high power demand (high and mid lines) corresponds great left/right load unbalance causing ipsilateral joint overload, at high neuromuscular coordination demand (low lines) corresponds great motor disorder causing uncontrolled motion. | |
Protocol: 6 pedalling modes with fixed power of 200 watt at changing frequencies and
handlebar grip:
|
|||
| Ese06 | Postural gait analysis | Inhibited posterior thigh muscles semimembranosus (SM), semitendinosus (ST), biceps
Motor disorder in the left stride: Left Ground contact: in this context left PM and PMI should be inhibited to facilitate left shoulder backward motion, their pathologic contraction results in visibly disharmonious shoulder motion; Left Flat Foot: pathologically inhibited TP action resulting in unstable and pronated ankle; Left Mid Stance: pathologically contracted TFL inhibits hamstring keeping pelvis in pathologic anterior tilt, resulting in low propulsion and poor balance; Left Heel Off: pathologic hamstring elongation secondary to pelvis anterior tilt requires early knee flexion resulting in early heel off, in this phase GM that should be providing propulsion but pathologically contracted TFL inhibits it, supplementary motion is supplied by S; Left Late Stance: early heel off and poor knee flexion due to pathologically inhibited hamstring result in vertical push off causing left hip adduction and poor propulsion; Left swing: previous phase (late stance) fails in delivering limb inertial angular velocity to swing pahase, limb enhancement is then actively taken over by frontal muscles (TFL, RF) and clearance is optimised by quadratus lumborum (QL) providing hip adduction, it all results in poor foot clearance and easiness in stumbling. In this context EHL and FHL co-contraction (Ese01) should provide big toe clearance, but pathologically inhibited FHL is not able to flex phalangeal joint, as such, big toe is straight extended by EHL inducing harmful pressure of the nail against the shoe and threatening its ingrowing. |
|
| Ese07 | Left thorax: motor disorder | Inverted rib expansion during inspiration: chest expansion for inspiration is compromised by anterior scalenus and intracostalis contraction (as well al PM and suspect pectoralis minor (PMI)) and is compensated by posterior expansion and augmented kyphosis resulting in dorsal expansion respiration. | |
| Ese08 | Tongue: motor disorder | Left unilateral tongue weakness (no apparent muscle loss): extraoral manifestation is a slight tongue deviation (Ecl20) assessable by GG contraction test as well, but the dramatic pharyngeal and intraoral consequences are upper airway patency loss (Ptd01), maxillary arch insufficiency (Ptd03) and swallowing disorder. Given the resulting functional limitation, tongue weakness is not confined to GG only but reasonably extend to hyoglossus (HG) and SG. Although GG contraction test may reliably assess genioglossus weakness, strength assessment on other extrinsic tongue muscles has to be otherwise performed. | |
| Ese09 | Mandible: motor disorder | Mandibular left mastication pattern disorder (right is physiologic): lateral-retrusive jaw motion with maxillary canine distal guidance instead of the physiologic lateral-protrusive with maxillary canine mesial guidance; the evaluation is performed after orthodontic treatment because in the pre treatment teeth crowding kept from canine and incisors guidance employment, hence, from physiologic mastication. | |
| Ese10 | Facial expression: motor disorder | Due to permanent cheeks activity in smile wise expression (Ecl23) impacting on mood and, according to context, resulting in social uneasiness, moreover, permanent orbicularis activity encourages upper incisors internal inclination; | |
| EVIDENCES: regression events | ||
| Postural symptoms are chronic, continuous, no memory of arising, present at lease since age 22, nevertheless they are reversible, this confidence is provided by regression events. Regression events are periods of unilateral postural symptoms partial but simultaneous subsidence, complete understanding of these regression events is challenging, these events have been of great help for developing the mechanics-pathomechanics-etiopathogenesys hypothesis. | ||
| # | Finding | Details |
| Ere01 | Regression extents | Regression events extents:
|
| Ere02 | Relationship | During true regression events the patient experiments a true subsidence of all the
unilateral postural disorder and some other symptom, physiologic motor
behaviour is restored, in this context the patient has been able to notice
that big efforts (eg. sport training) reduce the effect of the regression
event, in other words fatigue seems to trigger back unilateral motor
disorder. According to cause-effect relationship, regression events are subdivided into:
|
| Ere03 | Sensations | Sensations experienced during index 1 events:
|
| Ere04 | Subsided symptoms | Evidences experimenting subsidence during regression events: Ese01, Ese02, Ese03, Ese04, Ese05, Ese06, Ese07, Ese08, Ese09, Esy05, Esy07, Esy08. |
| EVIDENCES: orthodontic treatment, outcome and follow up | |||
| Evidences emerging from the initial kinesiologic diagnostic evaluation demonstrated dental occlusion disorder involvement in part of the patient postural deviation, unfortunately no direct evidence of relationship with the unilateral lamented symptoms emerged, despite this lack of confirm the orthodontic treatment has been decided to be worth undertaking. | |||
| # | Phase | Images & details | |
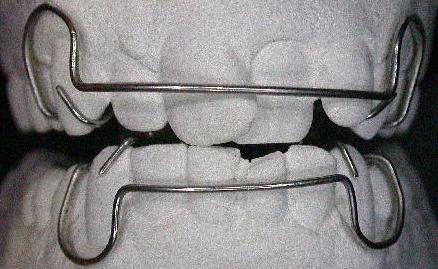
| Eot01 | Therapy | Orthodontic treatment:
|
|
| Eot02 | Outcome | Effects:
|
|
| Before/after:: | |||
| Eot03 | Subsided postural symptoms | Subsided symptoms per category:
|
|
| Eot04 | Newly onset symptoms | Esy06, Esy07. | |
| Eot05 | Follow up | 2 months after orthotic removal:
| |
| Eot06 | Restored symptoms | Ecl03, Ecl05, Ecl06, Ecl08, Ecl12, Ecl14, Ecl19, Esy03, Esy04, Esy08. | |
| Eot07 | Subsided symptoms | Esy07 (improved but not subsided). | |
|
Bugs report and technical issues notification to the webmaster are highly apreciated
|
| Posture, etiology of a syndrome - ©2008 Paolo Platania |















 click to enlarge
click to enlarge